What is Interlocking Nail Implant and How Does It Work?
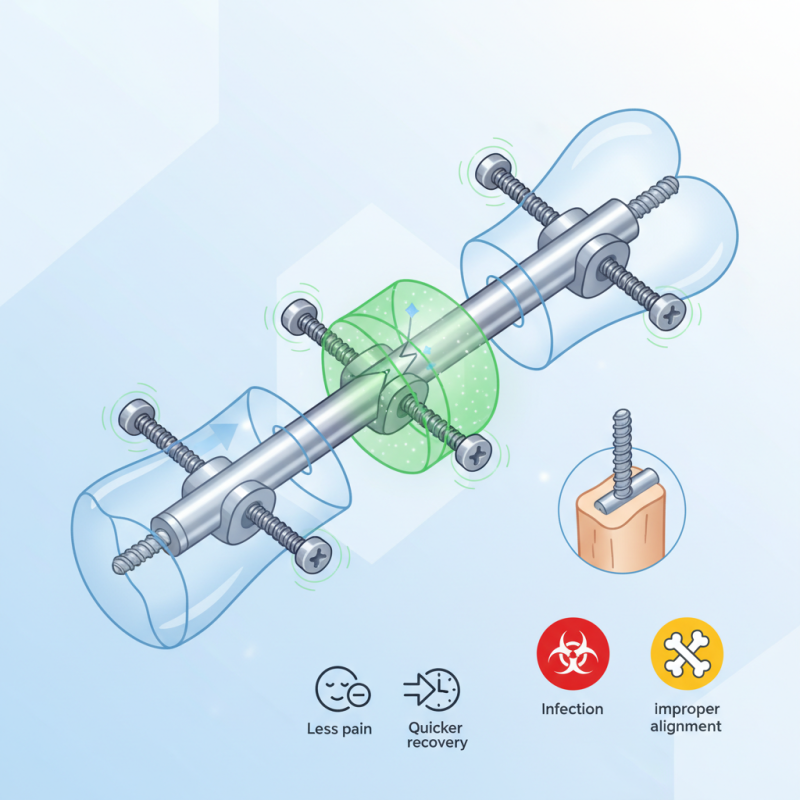
The Interlocking nail implant is a groundbreaking tool in orthopedic surgery. This innovative device plays a vital role in stabilizing and uniting broken bones. With its unique design, it allows for secure fixation within the medullary canal of long bones.
Surgeons use the Interlocking nail implant for various fractures, particularly in the femur and tibia. Its interlocking mechanism ensures that the bone fragments remain properly aligned during the healing process, facilitating quicker recovery. Patients often experience less pain and mobility restrictions compared to traditional fixation methods.
However, the application of the Interlocking nail implant is not without challenges. Surgeons must carefully assess each case to ensure an appropriate fit. Complications can arise, including infection or improper alignment. These potential issues highlight the need for continued reflection and improvement in surgical techniques and patient care.
What is an Interlocking Nail Implant?
Interlocking nail implants are innovative devices used in orthopedic surgery. They provide internal fixation for long bone fractures. The design allows them to lock in place, enhancing stability. This method is particularly effective in treating complex fractures.
The implant is inserted through both ends of the bone. It connects the proximal and distal parts of the fracture. Studies show that interlocking nails can lead to a 90% union rate among patients. This statistic highlights their effectiveness in promoting healing. The procedure is minimally invasive, reducing recovery time for many patients.
Despite their benefits, there are challenges. Some patients experience complications, like infection or implant failure. Reports indicate that approximately 10% of patients may face these issues. Surgeons must carefully assess each case to determine suitability. This decision-making process is crucial for achieving desired outcomes.
The Engineering Behind Interlocking Nail Implants
Interlocking nail implants represent a significant advancement in orthopedic surgery. These devices play a crucial role in stabilizing long bone fractures. The design features a metallic nail that is inserted lengthwise into the bone. It offers a robust internal fixation. The interlocking system uses screws that engage in pre-drilled holes, providing added stability.
The engineering behind these implants is fascinating. The nails are crafted from biocompatible materials, ensuring they coexist peacefully with body tissues. The precision in manufacturing is vital. Even slight imperfections can lead to complications. Surgeons must pay close attention to alignment during implantation. The goal is to hold the fractured ends closely together. This promotes healing and restores function.
Challenges remain in this technology. Surgeons need extensive training to master the insertion technique. Misalignment can affect the healing process. Additionally, there's a risk of infection or complications from foreign materials. As the field advances, continuous improvements in design and technology are essential. Each innovation brings new opportunities for better surgical outcomes.
How Interlocking Nail Implants Are Inserted
Interlocking nail implants are essential in treating certain fractures. The insertion process involves several steps that require precision. Initially, the surgeon prepares the area. They assess the fracture and determine the optimal entry point. It's crucial to align the nail with the bone.
Once the site is ready, the procedure begins. An incision is made at the fracture site. Then, the surgeon drills a hole into the bone. This step is delicate. It must be done carefully to avoid damaging surrounding tissues. After the initial drilling, the interlocking nail is inserted. The nail is designed to stabilize the fracture effectively.
Alignment is key during insertion. The implant should fit snugly within the bone. Surgeons often use fluoroscopy to guide them. This imaging technique helps ensure correct placement. After the nail is in place, locking screws are added. They provide additional stability.
Despite the advances in technology, complications can occur. Inadequate alignment can lead to healing issues. It’s important for patients to discuss potential risks upfront.
Benefits of Using Interlocking Nail Implants for Fracture Repair
Interlocking nail implants have gained popularity for repairing bone fractures. They work by being inserted into the medullary cavity of the bone. This device stabilizes fractured bones and allows for better healing. Surgeons use these implants for diaphyseal fractures most effectively.
The benefits of interlocking nail implants are significant. They provide excellent stability, allowing patients to regain mobility faster. Patients often experience less pain compared to traditional methods. The technique minimizes soft tissue damage, promoting quicker recovery. On the downside, not all fractures are suitable for this treatment. Some unique cases may lead to complications that require further interventions.
Moreover, a learning curve exists for surgeons. Precision in placement is crucial. If the nail is not positioned correctly, it can lead to malunion or delayed healing. This highlights the importance of skillful execution. While the advantages are compelling, the potential risks should not be overlooked. Each case needs thorough evaluation before choosing this method.
Recovery and Rehabilitation After Interlocking Nail Surgery
Recovery after interlocking nail surgery can be a complex process. Patients often experience pain, swelling, and discomfort. These issues can persist for several weeks. According to a study published in the Journal of Orthopedic Surgery, about 30% of patients report significant pain during the initial recovery phase. This can be discouraging and may require additional pain management strategies.
Rehabilitation is crucial for regaining mobility and strength. Physical therapy often starts within a few days post-surgery. Early mobilization can help prevent stiffness and improve joint function. A report by the American Academy of Orthopaedic Surgeons indicates that approximately 70% of patients show substantial functional improvement after a structured rehabilitation program. However, not all patients follow their rehab plans. Adherence can drop due to discomfort or lack of motivation.
As recovery progresses, regular follow-ups with healthcare providers are important. They can monitor healing and adjust rehabilitation plans. Patients should be aware of the signs of complications, such as increased swelling or fever. Maintaining a proactive approach enhances overall recovery. It's essential to understand that healing takes time; the process can be frustrating, but patience is necessary for long-term success.